US health insurance
#211
Forum Regular




Joined: Jul 2018
Location: California
Posts: 254











The system is complicated and it can be difficult to know what you're getting into when you choose a plan. I would ask Covered CA if it's possible to switch to a different plan straight away; if not, and this continues to be a hassle, you have till the end of January to switch to another plan starting 1st February.
#212
The system is complicated and it can be difficult to know what you're getting into when you choose a plan. I would ask Covered CA if it's possible to switch to a different plan straight away; if not, and this continues to be a hassle, you have till the end of January to switch to another plan starting 1st February.
#213
My insurance woes described above seem to be settling down and I now appear to be covered for 2022 
I am now trying to schedule my 5-year colonoscopy (lucky me!). Before they will schedule me, they want me to sign an ton of forms, one of which contains this gem:
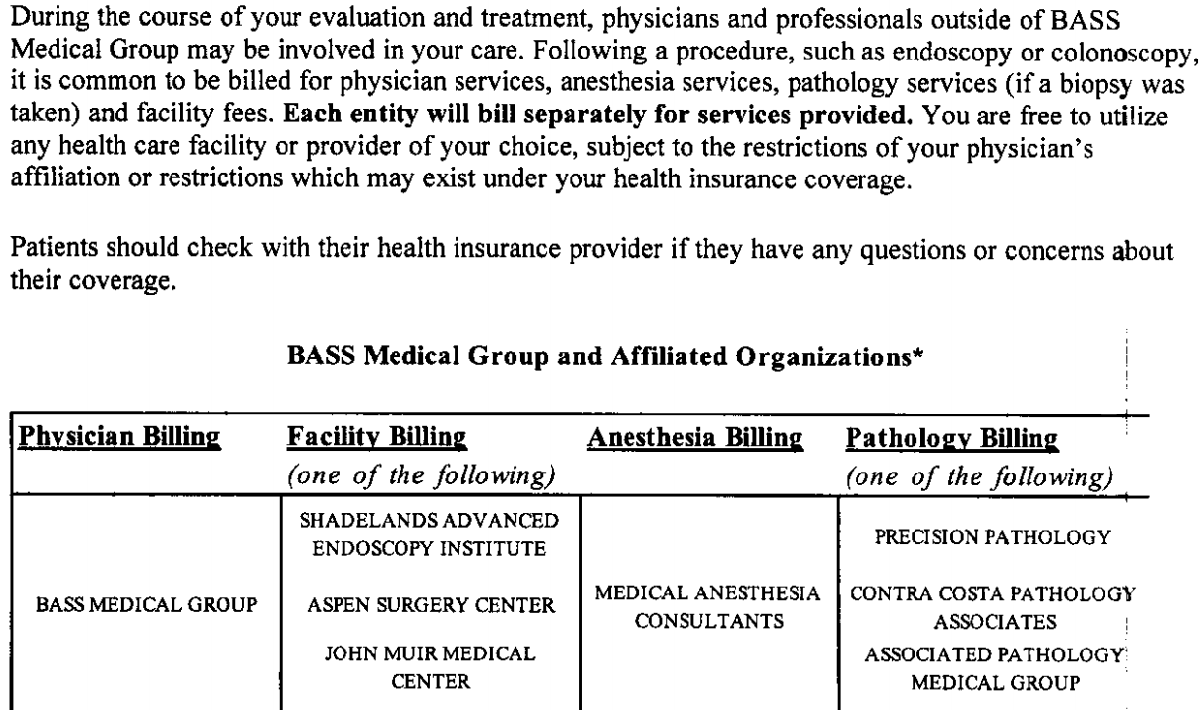
So they are saying multiple organizations will be involved (doctors, facilities, anesthesiologists, and pathologists), each of which will bill me separately, and ... I guess ... it's MY responsibility to find out which if any are covered by my insurance company. So does this mean I need to call the insurance company and ask if these organizations are covered? This seems incredibly burdensome. I'm now on an HMO plan, which is less flexible than my previous plans so I need to be more careful.

I am now trying to schedule my 5-year colonoscopy (lucky me!). Before they will schedule me, they want me to sign an ton of forms, one of which contains this gem:
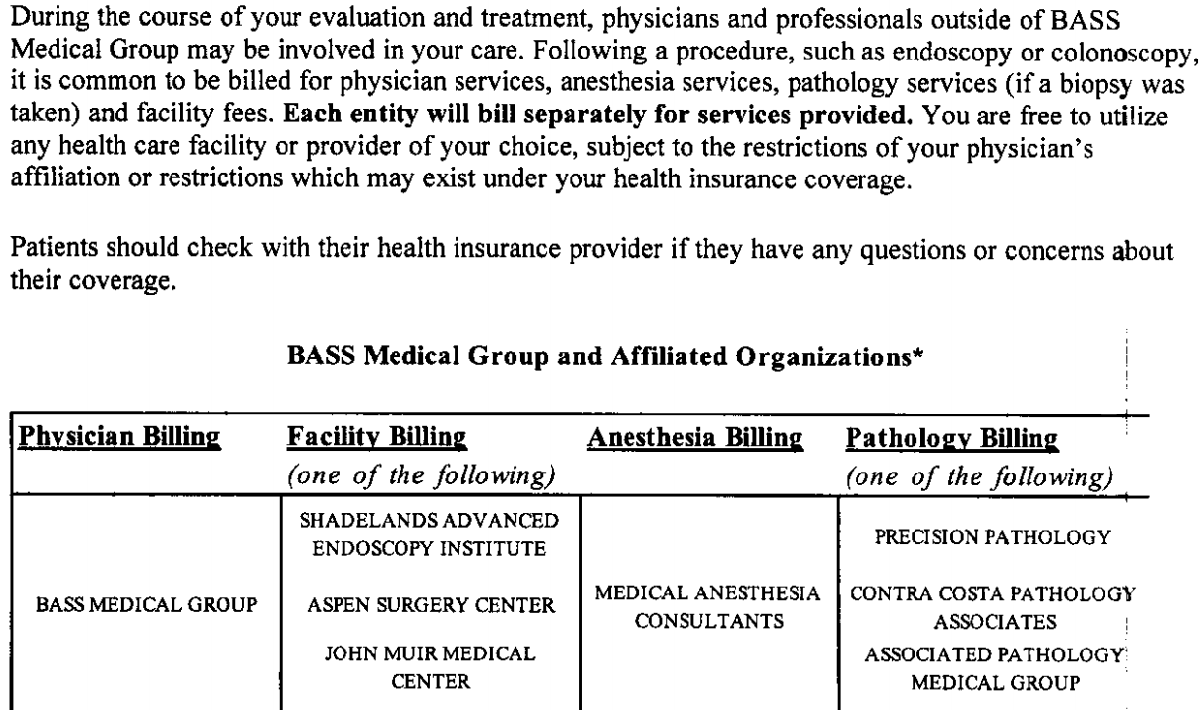
So they are saying multiple organizations will be involved (doctors, facilities, anesthesiologists, and pathologists), each of which will bill me separately, and ... I guess ... it's MY responsibility to find out which if any are covered by my insurance company. So does this mean I need to call the insurance company and ask if these organizations are covered? This seems incredibly burdensome. I'm now on an HMO plan, which is less flexible than my previous plans so I need to be more careful.
#214
That’s exactly what that means, and yes, it sure is burdensome. If even one of those is out of network, you’ll either have to stomach it, or start over again at another provider.
#215
BE Forum Addict







Joined: Aug 2013
Location: Athens GA
Posts: 2,134











At least they gave you a list of the other facilities that may be involved. In my experience I have never got anything like that.
#216
BE Forum Addict









Joined: Aug 2013
Location: Eee Bah Gum
Posts: 4,131











The last colonoscopy my wife and I had done I went through the same process, and checked that the facility, and doctor was in-network. After the bills rolled in we still got screwed because they used 2 different labs to test the polyps they incised and one of those labs was out of network. (Tests all came back negative which was good). We were billed $375 each for those lab tests and it took 12 months of appeals and aggro before the insurance company agreed to pay $20 each test and we paid an additional $30 each test. Would they have used only the 3 in-network labs if I had asked ahead of time? Who knows.
#217
Lost in BE Cyberspace










Joined: Jan 2006
Location: San Francisco
Posts: 12,865











My last colonoscopy ended up with me having the biggest fight I've ever had with my insurance, the doctor who performed it and other providers. After a ridiculous amount of effort I went from being asked to pay thousands, to paying virtually nothing.
#218
I agree.
The last colonoscopy my wife and I had done I went through the same process, and checked that the facility, and doctor was in-network. After the bills rolled in we still got screwed because they used 2 different labs to test the polyps they incised and one of those labs was out of network. (Tests all came back negative which was good). We were billed $375 each for those lab tests and it took 12 months of appeals and aggro before the insurance company agreed to pay $20 each test and we paid an additional $30 each test. Would they have used only the 3 in-network labs if I had asked ahead of time? Who knows.
The last colonoscopy my wife and I had done I went through the same process, and checked that the facility, and doctor was in-network. After the bills rolled in we still got screwed because they used 2 different labs to test the polyps they incised and one of those labs was out of network. (Tests all came back negative which was good). We were billed $375 each for those lab tests and it took 12 months of appeals and aggro before the insurance company agreed to pay $20 each test and we paid an additional $30 each test. Would they have used only the 3 in-network labs if I had asked ahead of time? Who knows.
Last edited by Steerpike; Feb 16th 2022 at 7:47 pm.
#219
Forum Regular

Joined: Apr 2019
Posts: 46











I spent the morning tracking some of this down; neither the Anesthesia group, nor the three Pathology groups, appear to be covered (although, they may go by different names - eg, 'BASS' was not listed, but 'Bay Area Surgical Specialists' was). So now I'm asking them for estimates of what it would cost me, and also, I'm asking my provider for another referral so I can explore alternatives. Normally I'd just pursue this slowly but I'm actually having some lower abdominal pain and other issues so I'm keen to get the colonoscopy done!
I had that same experience last time (5 years ago), which is why I'm being more pro-active this time about checking.
I had that same experience last time (5 years ago), which is why I'm being more pro-active this time about checking.
https://www.cms.gov/newsroom/fact-sh...-medical-bills
https://www.brookings.edu/blog/usc-brookings-schaeffer-on-health-policy/2021/02/04/understanding-the-no-surprises-act/
One of the provisions is to "Ban out-of-network charges and balance bills for certain additional services (like anesthesiology or radiology) furnished by out-of-network providers as part of a patient’s visit to an in-network facility."
"Starting January 1, 2022, it will be illegal for providers to bill patients for more than the in-network cost-sharing due under patients’ insurance in almost all scenarios where surprise out-of-network bills arise, with the notable exception of ground ambulance transport. Health plans must treat these out-of-network services as if they were in-network when calculating patient cost-sharing"
"Under the notice and consent process, an out-of-network provider must notify a patient of its out-of-network status and obtain the patient’s written consent to receive out-of-network services more than 72 hours before the service is delivered. The goal of such an exception is to allow patients who wish to do so to choose an out-of-network provider when a substantive choice exists. The law also establishes that there is no notice and consent exception allowed for services where patients are typically unable to select their specific provider. This “no exception group” is defined as any service relating to emergency medicine, anesthesiology, pathology, radiology, neonatology, diagnostic testing, and those provided by assistant surgeons, hospitalists, and intensivists."
Last edited by ss120396; Feb 19th 2022 at 12:14 am.
#220
This doesn’t really apply in this situation, since it is expressly why he was given the document breaking down the providers.
Hard to call it a surprise bill when they have given him the chance to find out in advance.
Hard to call it a surprise bill when they have given him the chance to find out in advance.
#221
Forum Regular

Joined: Apr 2019
Posts: 46











https://www.cms.gov/files/document/s...g-consumer.pdf
Last edited by ss120396; Feb 19th 2022 at 7:16 am.
#222
Yes that's a form that the patient would usually sign on admission. Most people won't even read it.
#223
Forum Regular

Joined: Apr 2019
Posts: 46











That said, it looks like they took precautions in drafting the law to avoid the situation you described. Pages 1-2 of the form:
"The standard notice and consent documents must be given physically separate from and not attached to or incorporated into any other documents. The documents must not be hidden or included among other forms, and a representative of the provider or facility must be physically present or available by phone to explain the documents and estimates to the individual, and answer any questions, as necessary"
"If an individual makes an appointment for the relevant items or services at least 72 hours before the date that the items and services are to be furnished, these notice and consent documents must be provided to the individual, or the individual’s authorized representative, at least 72 hours before the date that the items and services are to be furnished. If the individual makes an appointment for the relevant items or services within 72 hours of the date the items and services are to be furnished, these notice and consent documents must be provided to the individual, or the individual’s authorized representative, on the day the appointment is scheduled. In a situation where an individual is provided the notice and consent documents on the day the items or services are to be furnished, including for post-stabilization services, the documents must be provided no later than 3 hours prior to furnishing the relevant items or services."
Last edited by ss120396; Feb 19th 2022 at 7:51 am.
#224
I assume you are familiar with the concept of online check in? Unless receiving emergency services, a significant number of people, at least in experience at my own facility, electronically sign in prior to attending the facility - thereby meeting the 72 hour required.
I don't mean to suggest that this isn't a god thing, of course it is, but it will still happen. Unfortunately the people it will still happen to are those that either do not read the form, or are not aware of the changes in the law. Which are likely to be the demographic that are least likely to be able to afford it and consequently are most likely to default on payment - which results in unreimbursed care which ends up costing all of us more.
I don't mean to suggest that this isn't a god thing, of course it is, but it will still happen. Unfortunately the people it will still happen to are those that either do not read the form, or are not aware of the changes in the law. Which are likely to be the demographic that are least likely to be able to afford it and consequently are most likely to default on payment - which results in unreimbursed care which ends up costing all of us more.
#225
I would look into the new federal law that went into effect this year, the "No Surprises Act", to see how it might apply here.
https://www.cms.gov/newsroom/fact-sh...-medical-bills
https://www.brookings.edu/blog/usc-brookings-schaeffer-on-health-policy/2021/02/04/understanding-the-no-surprises-act/
One of the provisions is to "Ban out-of-network charges and balance bills for certain additional services (like anesthesiology or radiology) furnished by out-of-network providers as part of a patient’s visit to an in-network facility."
"Starting January 1, 2022, it will be illegal for providers to bill patients for more than the in-network cost-sharing due under patients’ insurance in almost all scenarios where surprise out-of-network bills arise, with the notable exception of ground ambulance transport. Health plans must treat these out-of-network services as if they were in-network when calculating patient cost-sharing"
"Under the notice and consent process, an out-of-network provider must notify a patient of its out-of-network status and obtain the patient’s written consent to receive out-of-network services more than 72 hours before the service is delivered. The goal of such an exception is to allow patients who wish to do so to choose an out-of-network provider when a substantive choice exists. The law also establishes that there is no notice and consent exception allowed for services where patients are typically unable to select their specific provider. This “no exception group” is defined as any service relating to emergency medicine, anesthesiology, pathology, radiology, neonatology, diagnostic testing, and those provided by assistant surgeons, hospitalists, and intensivists."
https://www.cms.gov/newsroom/fact-sh...-medical-bills
https://www.brookings.edu/blog/usc-brookings-schaeffer-on-health-policy/2021/02/04/understanding-the-no-surprises-act/
One of the provisions is to "Ban out-of-network charges and balance bills for certain additional services (like anesthesiology or radiology) furnished by out-of-network providers as part of a patient’s visit to an in-network facility."
"Starting January 1, 2022, it will be illegal for providers to bill patients for more than the in-network cost-sharing due under patients’ insurance in almost all scenarios where surprise out-of-network bills arise, with the notable exception of ground ambulance transport. Health plans must treat these out-of-network services as if they were in-network when calculating patient cost-sharing"
"Under the notice and consent process, an out-of-network provider must notify a patient of its out-of-network status and obtain the patient’s written consent to receive out-of-network services more than 72 hours before the service is delivered. The goal of such an exception is to allow patients who wish to do so to choose an out-of-network provider when a substantive choice exists. The law also establishes that there is no notice and consent exception allowed for services where patients are typically unable to select their specific provider. This “no exception group” is defined as any service relating to emergency medicine, anesthesiology, pathology, radiology, neonatology, diagnostic testing, and those provided by assistant surgeons, hospitalists, and intensivists."
I have told them none of the providers are in my insurance company's 'network'. I also did not sign the form (though, they may ask me to sign again closer to the time of the procedure; and if they wait until 'the day of', then I'm within the 72 hours so I'm in good shape). They did say that they would run an insurance 'pre-approval' with my insurance company, but they won't do that until 1 week prior, which doesn't give me time to find an alternative gastroenterologist. If they run the pre-approval and my ins. co. says 'not approved' for (eg) Anesthesiologist, I will try to raise an issue that - I'm in an HMO plan, and as part of an HMO plan, I'm not allowed to choose my own providers; I have to go with the direction of both my PCP (for a referral) and my 'IPA' (Individual Practice Association) - the 'medical group' that my PCP belongs to, and that is supposedly contracted to deliver all my HMO care. When an insurance company assigns or 'approves' an IPA to be in their network, I get the impression that IPA has to follow the rules of the HMO in that, everything they arrange and approve for my 'care' must be 'in network'. Similarly, when the ins. co. approves the gastroenterologist to be 'in network', and it's an HMO, I wonder if he is not obligated to only provide 'in network' services.
I tried to get my PCP to give me a second referral, so I could see whether a different gastroenterologist would have a more appropriate set of 'associates', but he was pretty dismissive of my request (I used the 'messaging' system I have with the doctor, which is not very good). I may ask him again. But my current instinct is to go ahead and get it done, and then fight like hell after the fact based on all the various factors above - in part because I feel a sense of urgency in getting it done, and in part because I'm curious to see how it turns out.
Edit to Add:
Regarding this sentence specifically from the excerpt above: "Under the notice and consent process, an out-of-network provider must notify a patient of its out-of-network status and obtain the patient’s written consent to receive out-of-network services more than 72 hours before the service is delivered."
In my case, there are multiple 'providers' and it's not clear how exactly I should interpret this.
My main 'provider' is the GE (GastroEnterologist). He's in network, and has been approved by my insurance already.
The Anesthesiologist is also a 'provider', I believe, in the context of the above excerpt. But I'm not being presented with any paperwork by the Anesthesiologist, so 'he' is not notifying me. Only the GE has asked me to sign a form that is generally waiving my rights. And he's also saying, in that document he wants me to sign, that "I'm free to choose any provider I choose ...". So if I ask him to use an Anesthesiologist that is in my network, he should comply.
Last edited by Steerpike; Feb 20th 2022 at 4:45 am.



